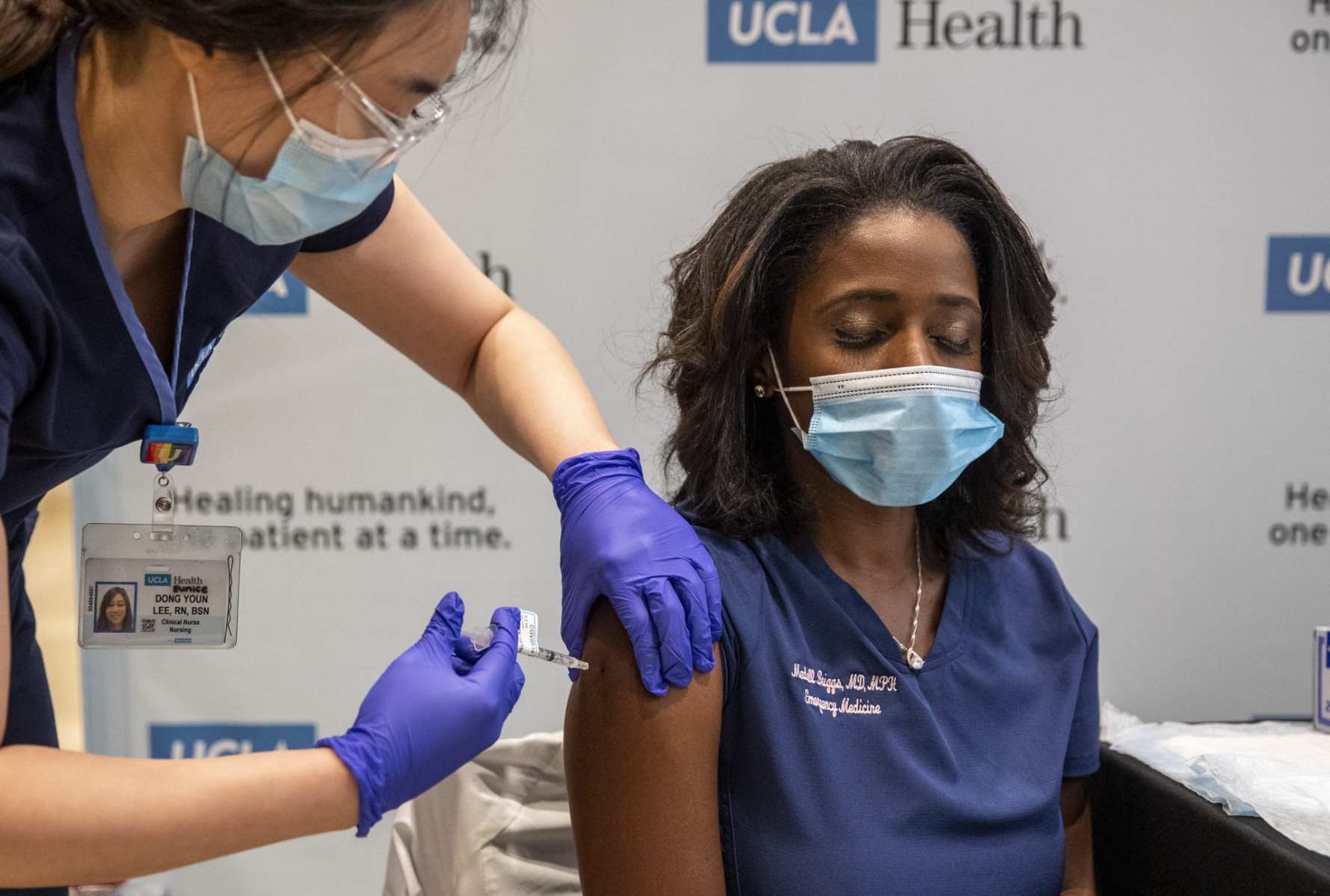
The nascent coronavirus vaccine rollout is offering the nation’s majority-women health care workforce a first glimpse of relief from the brutal pandemic.
The nation’s 21 million health care workers, 75 percent of whom are women, are in the first wave of Americans to receive Pfizer’s COVID-19 vaccine, which was authorized for emergency use last weekend. The Food and Drug Administration is expected to grant a similar authorization Friday for a second vaccine, produced by Cambridge, Massachusetts-based Moderna.
Health care workers told The 19th that the potential for a vaccine offers them some desperately needed hope. But it comes just as the devastating rise in cases — now more than 300,000 people are dead and hospitals across the country are running low on ICU beds — threatens once again to overwhelm the health system, as well as the women who power it.
Women on the frontlines say they’re feeling a mix of emotions — there’s hope, but also exhaustion and burnout from the past few months. And there’s nervousness and uncertainty about what, even with the vaccine, the coming winter months, which are forecast to be some of the pandemic’s deadliest, will look like.
“We haven’t had good news so far. It’s always been bad news after another. Every month it’s getting worse,” said Helena Sarai Cobos, a hospitalist physician at McAllen Medical Center in South Texas, which has emerged as a coronavirus hotspot. The vaccine “is a little light at the end of the tunnel.”
States, counties and hospitals will have to determine which health care workers are the first to get immunized, using a limited supply of vaccines on the people who are theoretically most likely to be exposed to the coronavirus at work. At least initially, there are enough vaccines to immunize about 20 million people, with those first immunizations being shared between the 21 million health care workers and the nation’s 3 million nursing home residents.
Both Pfizer’s and Moderna’s vaccines are administered over two shots, given three or four weeks apart. Evidence suggests they are more than 90 percent effective in protecting people from the virus.
Meanwhile, public health experts warn that the new surge in cases means the coronavirus death count could surpass 400,000 by the end of February. Even though health care workers are getting immunized now, experts are predicting the vaccine won’t be available to the general healthy public until spring, likely March or April.
If more Americans adhere to social distancing recommendations and wear masks, it’s still possible to curb the virus’ spread, experts say. But many health care workers said they’re worried that the news of the vaccine, combined with pandemic fatigue, will result in more people abandoning any precautions. (Public health officials have been urging Americans to adhere strictly to mask-wearing and social distancing in the coming months, especially on the heels of the vaccine news.)
“It’s the first time I’ve felt hopeful any time in months,” said Jessica Goddard, a 28-year-old medical resident in Pittsburgh, who has been working on her hospital’s COVID unit and expects to be vaccinated in the next few weeks. “I think that it’s just important to keep in perspective that it’s still going to be a while before we see the results of this. It’s not going to go away overnight when people get vaccinated.”
Already, health care workers are stretched thin. Last weekend, Goddard said, her hospital briefly ran out of ventilators, which are used to help severely ill coronavirus patients breathe. They had to temporarily borrow more machines from the nearby children’s hospital.
She has no doubt things will get worse. But, still, she said, she can’t look too far to the future, or begin to think about what January or February will look like.
“You want to have a plan, but we’re already at Plan Z. We don’t have plans beyond this,” she said. “Knowing this eventually will end, and the vaccine is the first step in that process of getting back to any realm of normalcy — it’s reassuring. But sometimes it’s hard to be hopeful when you’re right in the thick of everything.”
The last several months have imposed their own heavy psychological strain. Cobos, who has lived in South Texas for 15 years, said she has treated familiar faces, including her friends’ relatives, and seen her coworkers contract the virus. Some haven’t survived.
“It’s been very stressful,” she said. “It’s tough, especially when you are a community member and have relatives and friends in the region.”
Even as the vaccine rolls out, gaps in the system remain, creating uncertainty for many workers. Take the nation’s traveling nurses, who have emerged as a critical resource for overwhelmed hospitals, and who are estimated to account for close to 50,000 nurses nationwide.
Because Amy Consolatore, a travel nurse, contracts through an agency and doesn’t work for a single hospital, she doesn’t know when she will get vaccinated. Since March, the 32-year-old nurse from Daytona, Florida, has traveled to care for COVID-19 patients in Connecticut — just an hour outside of hotspot New York City — and Seattle. She’s planning to go to Texas in January, she said, which has had more than 1.5 million total cases of the virus reported, and saw almost 22,000 new cases on Wednesday.
“I’ve learned by necessity some ways to manage my anxiety, and it’s still not enough,” Consolatore said. “I’m definitely burned out.”
She’s thankful the vaccine is coming, and believes that having more health care workers immunized will be invaluable, especially if the predicted winter surge materializes. But predominantly, she said, she feels tired, frustrated and ignored, especially by friends and relatives who still don’t believe the pandemic is real. Getting vaccinated doesn’t undo that exhaustion, which she says many of her colleagues share.
“When I was in Connecticut, every day I went to work, I was like, ‘I haven’t gotten a single patient off the ventilator at all, not one.’ … That’s a lot of patients that I haven’t seen live,” she said. “My own family is out there right now going to church without masks. It’s hard to feel that disrespected.”
Meanwhile, people who are currently pregnant or breastfeeding — about 330,000 of the health care workforce, per government estimates — have to navigate another layer of uncertainty. Neither Pfizer nor Moderna’s vaccine was tested among people who are pregnant or lactating. The federal government has said that health care workers who fit in that category can and should make the decision for themselves, in consultation with their own doctors, about whether they want to take the new immunizations.
It isn’t an easy decision. Mary Grady, a pediatric emergency room doctor in North Carolina, plans to get vaccinated sometime in the coming weeks. She’s nervous. Grady, 37, is breastfeeding her three-month-old infant.
“I have to balance the fact that, if I get COVID and bring it home, I could bring it to my family, or to my daughter or to my parents,” Grady said. “Does the benefit of a potential vaccine outweigh the risk of something that’s not been studied in our population?”
Theoretically, she said, she believes the risk from getting the vaccine is probably low — a point medical experts have also been making for months. And cases of coronavirus are climbing in her hospital, both in the general emergency department and the pediatric one where she works. At any given time, at least a few of her colleagues are probably quarantining and awaiting test results to see if they’ve contracted the virus.
“We don’t have enough providers to see patients,” she said. “Every day, I hear about new people having COVID. I feel like it’s only a matter of time before I have it, too. The vaccine cannot come soon enough.”
Meanwhile, authorities are still figuring out what vaccine distribution will look like after health care workers are immunized. The CDC is expected to recommend that “essential workers” be the next priority for vaccines, but the definition of “essential” isn’t set in stone. Because there isn’t a single federal vaccine distribution strategy, states are crafting their own plans to decide which such workers will qualify first.
Then there are money concerns. The Department of Health and Human Services has freed up about $340 million for states to distribute vaccines, and Congress is currently debating allocating another $6 billion as part of its December stimulus package. That’s still short of the $8.4 billion that the Association of State and Territorial Health Officials, which represents state-based health departments, say is needed.
Meanwhile, about a quarter of Americans say they probably or definitely still wouldn’t get a coronavirus vaccine, even if it is deemed safe by scientists and available for free. Many point to worries about potential side effects, and concerns that the vaccine development was rushed because of political pressure.
Concern about that skepticism inspired Laura Dean, a 32-year-old emergency medicine resident at Boston-based Mass General Brigham, to post a picture on Instagram when she got her first vaccine dose. Dean, who is currently breastfeeding her infant son, had been inactive on social media since she gave birth this spring, but she felt it was important to send a message.
“I felt compelled to say, ‘I’m a doctor, I’m breastfeeding, and it’s important. Let me add my voice to the people saying this is the right, smart, sensible thing to do,’” she said. “The risk of getting sick now and exposing my family is too great.”
Until there is a plan and resources to vaccinate the rest of the country and take other measures that tamp down the virus’ spread, Cobos said she worries about what it will take to develop the kind of immunity needed to bring real relief — for health care workers, and for the nation at large.
“It’s going to take a long time to produce herd immunity,” she said. “We have to immunize a large population, and that would take logistics.”